How CBT Heals
BASE was founded on the principles of Cognitive Behavioral Therapy (CBT) for one key reason: it is the most empirically validated psychotherapy. CBT was initially developed by Aaron Beck, MD, after he found that the common approach of psychotherapy did not demonstrate consistent outcomes. He utilized study of the experience of mental illness, specifically depression, and how therapy addressing the cognitions associated with depression could create meaningful change in depression. Prior to Beck, the dominant approach was psychoanalysis, which put the provider in the position of interpreting experiences for patients, who were viewed as incapable of understanding their own condition. Through his work, Beck was able to define specific commonalities in thoughts, emotions, and behaviors amongst people who had depression, and also discovered that changing these thoughts, emotions and behaviors brought about meaningful improvements in depression. Biggest change of all, Dr. Beck felt that therapists should take a coaching stance with their patients, rather than holding onto a position of power.
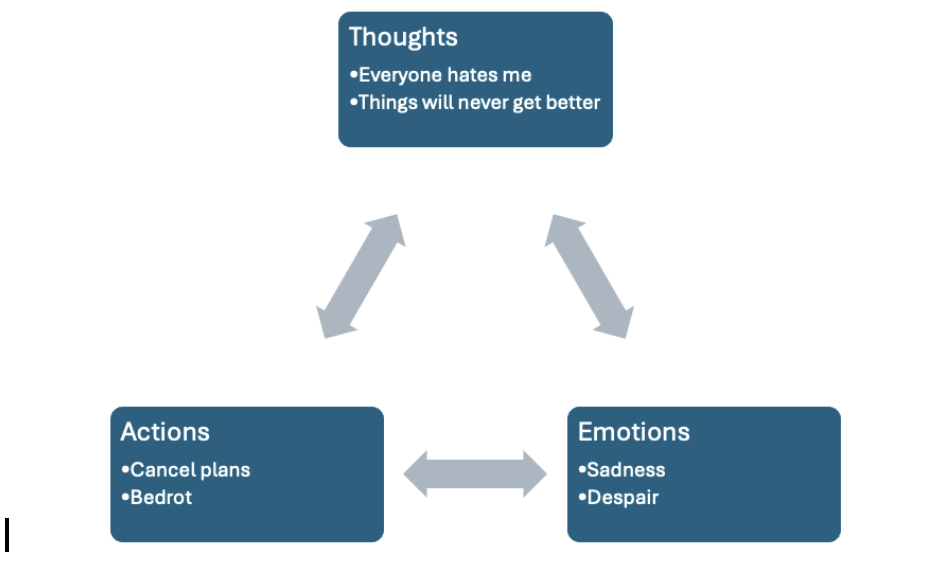
The CBT model of depression looks like the following:
Notice the arrows point in both directions, because each of these domains (thoughts, actions, emotions) can influence each other. For some people, depression might first start with diminished activities, which then leads to low mood and negative thoughts. For others, negative thoughts may lead to negative moods, which then results in diminished activity. The treatment of depression from a CBT lens involves intervention in each of the thoughts, moods, actions layer of the model. For many, changing behavior is a good starting point, but there is much that can be done for intervening at each level of the CBT depression model.
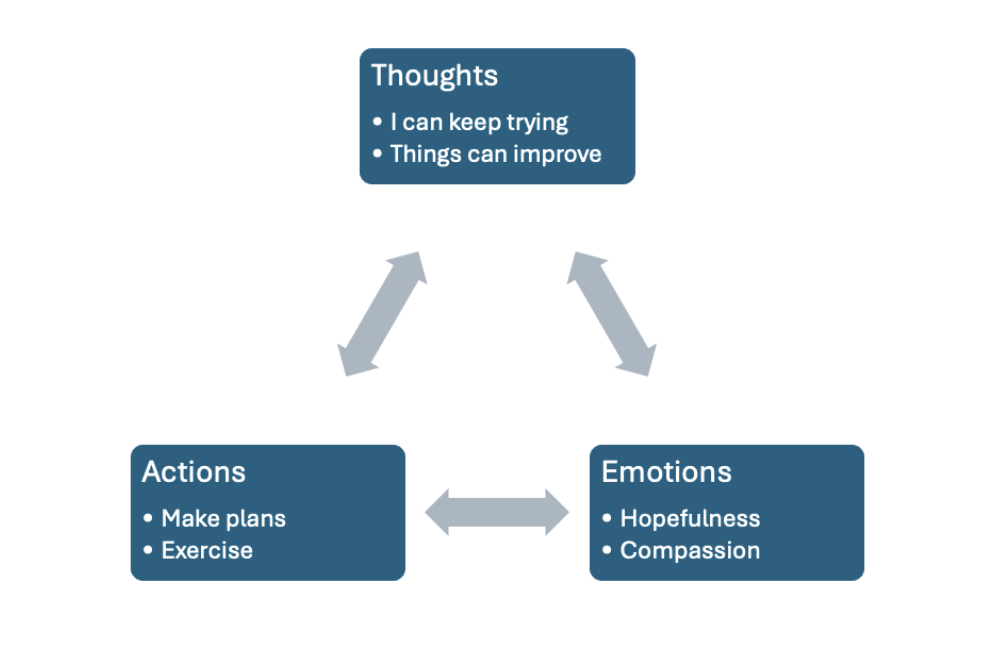
Treatment looks like this:
I usually like to start with actions, because they are easier to observe and measure. What thrills me about this work is the fact that engaging with it not only reduces symptoms in the short-term, but creates the capacity to change the neurological cause of the condition. For example, adding full-spectrum light exposure as a part of intervention increases serotonin, which reduces depression. Exercise affects several neurotransmitters that are part of depression and anxiety. In CBT for insomnia, brain imaging has demonstrated that the treatment increases production of the neurotransmitter GABA (the decrease of which is a cause of insomnia) and these increases are sustained well beyond the end of treatment. Exposure work in anxiety treatment reduces the anxious response, and can even decrease vulnerability to anxiety and panic. The action plans that are key to CBT are consistent with how the brain heals during treatment.
Over the past 50 years, CBT has been used to create manualized treatments for many psychological disorders, and continues to be a treatment with the strongest scientific evidence. From the start, CBT treatment focuses on the present moment, and treatment may end with movement toward healthier thoughts, emotions, and actions. CBT training manuals often present specific CBT interventions in 6-12 sessions, which are meant to make treatment accessible in clinics where the work needs to be focused on a specific goal. One of my first jobs after graduate school involved delivering CBT for people with chronic tinnitus, and our work always focused on tinnitus resolution, without much depth on greater personal issues. For this reason, there has been a pretty strong misconception that CBT is only a brief intervention that does not allow for people to understand their past experiences or fully heal. It is a pretty common misconception, and it completely misses the deep value of CBT.
As a professor for CBT at the Atrium Psychiatry Residency program, I focus on teaching CBT from a transdiagnostic perspective, meaning that any struggle can be evaluated from the perspective of problemating thoughts, emotions, and actions, and then treated by developing thoughts, moods, and actions that would move people in a positive direction. In private practice and the residency program, we are not limited to only 6-12 sessions, so we don’t have to skim the surface, and are able to engage with greater depth through treatment. Once you have engaged in understanding thoughts, emotions and behaviors, and have developed some movement out of psychological pain, we get to move to a deeper part of CBT treatment. We can look at life experiences and how they created emotional laws (called schema) which made us vulnerable to our maladaptive thoughts and emotions. We get to decide whether or not we want to perpetuate these emotional laws, or whether we would like to develop alternatives that support wellbeing for the long term. Lastly, we focus on how to reduce future vulnerability to struggles, and building a life worth living. Relearning new patterns can take a really long time, but also is one of the most rewarding parts of the work that we do. I honestly feel that I am incredibly lucky to be able to walk people through positive change, and to support bouncing back from the challenges life throws at them. The newer wave CBT therapies, ACT and DBT, also provide additional tools for going deeper into self understanding and specific steps for developing meaningful life paths.
For the month of February, the BASE team is going to be presenting on social media about the misunderstandings that they encounter in their area of specialization. BASE is committed to educating the public and other professionals about treatments that have a scientific foundation and strong evidence to their effectiveness. From the neurobiology of behavior change to the rewriting of emotional laws, CBT heals.
Looking for help through CBT? Get started below!